The Overactive Brain
Michela Gallagher was studying aging in lab rats when an unusual finding launched her on a translational journey that now sees her poised to initiate a Phase III trial of a drug to delay the onset of Alzheimer’s dementia.

In some ways, I’ve always been a neuroscientist – I was always very interested in memory and I became fascinated by the frequency and commonality of memory loss as people age. Today, my work lies at the intersection of normal age-related changes in memory, the pre-dementia state known as amnesic mild cognitive impairment (aMCI) and the full-blown symptoms that we recognize as dementia. Alzheimer’s doesn’t develop overnight – it’s an exceedingly slow progression from normal aging to dementia. The transitional phase of aMCI in which memory impairment is somewhat greater than expected for a person’s age can last a decade before progression to the point of a clinical diagnosis of early Alzheimer’s dementia.
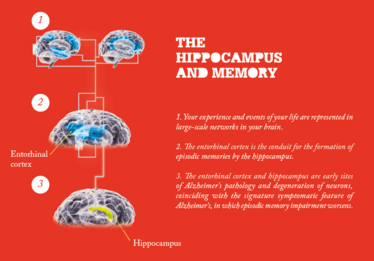
I didn’t set out to study Alzheimer’s disease. My work in this field hinges on a surprising finding from our studies on memory loss in aging rodents. In rats with memory loss, a subset of neurons critical for memory in the hippocampus are overactive. Other researchers made the same observation in patients with aMCI. This happens to some extent in normal aging but when Alzheimer’s pathology begins to emerge, hippocampal hyperactivity is driven higher and higher. Initially, it was thought that this might be a compensatory mechanism – the neurons working harder to try to hang onto making memories and overcoming damage. But our work in rats told us that this wasn’t true. To find out what the functional significance was, we had found ways to bring the activity down to normal levels. The result was to improve the memory deficits usually seen in those animals, suggesting that overactivity was causing rather than compensating for damage.
To translate the work into human patients, we needed to find a drug with a good safety profile that would dampen the overactivity in these neurons. After much searching, we found that levetiracetam – an FDA-approved and commonly prescribed atypical anti-epileptic – fitted the bill. Our initial studies in animal models and later in patients with aMCI have shown proof of concept and efficacy, with aMCI patients performing better in memory tests after treatment (2). Now, we have approval to start a larger-scale Phase III randomized clinical trial – HOPE4MCI - treating patients with aMCI with a low-dose, extended-release form of levetiracetam for 18 months (3). We’re still in the planning stages but we hope to start recruiting patients in 2016. We are using a dose of levetiracetam 12-times lower than that used in epileptics, so toxicity is not a major concern, but this is the first drug to attempt to slow the progression of aMCI into Alzheimer’s dementia by reducing overactivity in the brain.
Most clinical trials of Alzheimer’s therapies to date have involved people who already have a diagnosis of dementia, and almost all of those trials have failed. A few have an impact on symptoms, but at that stage of clinical dementia there is already a lot of irreversible damage in the brain. We’re trying to slow or stop neurodegeneration at an early phase of the disease, rather than reverse it. The Alzheimer’s Trajectory Report from the US Alzheimer’s Association suggests that a drug that could delay progression to a clinical diagnosis of Alzheimer’s disease by just five years would cut the prevalence of the disease by 40 percent and save the US economy over $300 billion.
It has been an amazing journey – from life as an academic scientist to founding a company and running a major clinical trial. I love science and making discoveries, and I find working with my students in the lab glorious; I often call the lab my playpen! The process of translation is sometimes a hard slog in comparison, but if we can make a difference to patients’ lives, it will be worth it.
Navigating the Complexity of Alzheimer’s
Untangling Tau by Brad Hyman
Food for Thought by Ewan McNay
Michela Gallagher is Krieger-Eisenhower Professor of Psychology & Neuroscience, Johns Hopkins University and Founder of AgeneBio, USA















