Cytotoxic Remediation
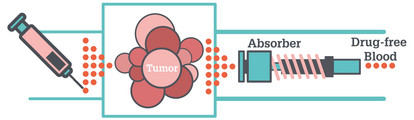
How a 3D-printed chemical absorber could pave the way for higher chemotherapy doses – or lower risks.
There is a challenge that oncologists have wrestled with for decades: how to provide patients with higher doses of cytotoxic drugs without potentially life-threatening toxicity. A 3D printed chemical absorber might provide the answer by “mopping up” excess cytotoxic drug before it enters the blood stream, according to a team based in the US (1). Here, we catch up with two of the researchers behind the device – Steven Hetts, Professor of Radiology at the University of California] and Nitash Balsara, Professor of Chemical and Biomolecular Engineering at UC Berkeley– for the background story and to learn their next steps.
Unmet need: the clinician’s story
Steven Hetts: As an interventional neuro-radiologist, one of the cancers I work with is retinoblastoma – a tumor of the eye that tends to occur in infants. We are able to use very powerful chemotherapy drugs because we are able to get the catheter right into the ophthalmic artery – the artery that goes right into the eyeball – so we are able to infuse very high concentrations. About half of the drug stays in the eyeball, but the other half passes through the veins in the eye and the face, and then circulates back to the heart through the jugular veins in the neck. Even that relatively small amount of chemotherapy often causes these infants to experience drops in their blood counts. And because the bone marrow is affected, they can get infections and anaemia.
Based on that experience, I said to myself, “Wouldn’t it be nice if there was a way to put a device next to the organ to drain or mop up excessive chemotherapy drug – and then remove it shortly thereafter so that the drug couldn’t re-elute?” I thought that such a device would minimize the systemic toxicity of the drug – at least, that was the original idea.
We decided to develop a device around a more common cancer – liver cancer – as it has tens of thousands of cases a year in the US, and hundreds of thousands of cases worldwide. The main drug used to treat it – doxorubicin – is a widely used agent that’s effective against many different cancers, but it suffers from dose-limiting toxicity. The main problem is heart failure – too much doxorubicin can cause cardiomyocytes to fail.
We wanted to develop a device that would bind doxorubicin in the hepatic veins – the major outflow from the liver – or the inferior vena cava. We spent a year in our lab, looking at different types of resins that might be able to bind to doxorubicin bionically, as well as a whole host of other approaches.
Applied solution: the chemical engineer’s story
Nitash Balsara: My group had initially been interested in polymers for battery application, which took us to the field of ionic polymers. It turns out that doxorubicin has an ionic character, and that the polymers that Steve and his students were working on were ionic in nature. We quickly realized through our networks that the polymers that our two groups were working on were similar.
Steve needed something like a sponge that would mop up the chemotherapy drug and that could be placed in a vein. Now, it clearly couldn’t be something exactlylike a sponge – a sponge would block the flow of blood as well. As a chemical engineer, I looked at the problem from a different viewpoint by imagining doxorubin was a pollutant. We routinely build absorption columns for pollutants such as sulfur in petroleum – these are the giant columns you see in an oil refinery. Our job then, was to design an absorption column that would function in the blood vessel.
The question was how do we build it? Luckily for us, 3D printing has become a science – rather than an art. We were also lucky to have access to a leading 3D-printing company in the San Francisco bay area – CARBON. Once our column was built, the next job was to coat the scaffold with a polymer that absorbed the drug. And that took a considerable amount of effort – the coating didn’t want to stick properly, and it wouldn’t apply itself uniformly. Fortunately, my post-doctoral student, Hee Jeung- Oh, learnt how to analyze the results and worked with the 3D printing company to fix the issue.
Now, we really feel that this design is what opens the door to the field, but we have no idea how big the room might be. We don’t know how much drug we might be able to absorb with these devices – the latest model is able absorb 64 percent of the administered drug (1).
Looking ahead
Steven Hetts: It’s exciting to think about how we could adapt the design in the future. Patients with tumors get PET and MRI scans, which generate 3D datasets; for example, a complete map of their venous anatomy. And so, beyond the initial generic 3D printed absorber, we could design a device that would fit perfectly into the vein of specific patient. This bespoke version would boost efficacy, because the drug would have no choice but to flow through the device. (Of course, there might be issues getting the device in there – we currently insert these devices using catheters – but it’s a surmountable challenge, I think!) In fairness, we’re a few years away from all that.
Based on other medical devices, it’s reasonable to think that after a more refined prototype has been proven safe in animal models, we will move onto human trials. The route from there obviously has several steps, but one of the nice things about devices like this – where you only insert them for a short period of time – is that they are much easier to test in terms of their safety and efficacy.
Our approach has broad potential – not just for chemotherapy drugs, but for other kinds of drugs or toxins. Our device could also have potential in more invasive procedures, such as dialysis and plasmapheresis. If you can work out the chemistry to do molecule binding, in situ – in the vasculature – you could open up many interesting opportunities.
- H J Oh et al., “3D printed absorber for capturing chemotherapy drugs before they spread through the body”, ACS Cent Sci Epub ahead of print. (2019)
















