Making Moves on Monkeypox
How is the world responding to the current global outbreak of monkeypox – and what are the challenges for widespread testing?
Olivia Gaskill | | 3 min read | Discussion
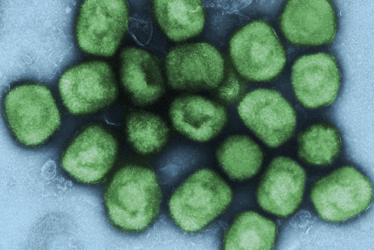
Credit: National Institute of Allergy and Infectious Diseases (CC BY 2.0).
As we gain footholds in the fight against COVID-19, we’re now watching a new disease – monkeypox – make its way around the world. SARS-CoV-2 was identified in 2019, but the first recorded human case of monkeypox was half a century earlier – so what is making the virus’ current spread so newsworthy and why is it spreading so quickly?
Though monkeypox is endemic in West and Central Africa, cases of the disease have now been detected in 27 non-endemic countries (and that number is steadily growing). The virus is usually spread through contact with an infected animal, but the latest outbreak is spreading via human-to-human transmission. Fortunately, monkeypox virus tends to mutate more slowly than SARS-CoV-2, making it less likely to evolve and find new ways to spread.
Testing troubles
Widespread testing has not yet been introduced in countries such as the US and UK – but, if the need arises, do governments and healthcare organizations have the structural capabilities and resources to implement such plans? To diagnose monkeypox, samples from the blisters and scabs are taken and sent to the lab for polymerase chain reaction (PCR) testing. Samples must be refrigerated (2–8°C) or frozen (-20°C or lower) within an hour of collection (1). Furthermore, monkeypox is a WHO Risk Group 3 pathogen, which requires laboratorians to handle samples with the utmost care and comes with specific guidance on who should perform testing.
“The smallpox vaccine is thought likely to prove at least 80 percent effective against monkeypox as they are closely related viruses. Here in the UK, we stopped regularly vaccinating against smallpox way back in 1971. Anyone under the age of 50 is unlikely to have been immunized,” said Quinton Fivelman, Chief Scientific Officer at London Medical Laboratory, UK (2). “America’s [CDC] says that, where possible, only vaccinated people (i.e., smallpox vaccination within the past 10 years) should perform laboratory work that involves handling specimens that may contain monkeypox virus. It says non-immunized people must use increased personal protection equipment and improved practices should be followed to further reduce the risk of exposure.”
Risk of misinformation
Since the first reported case of monkeypox outside West and Central Africa, Western media outlets have been reporting daily on its spread. But, if we hadn’t spent the last two and a half years living in a pandemic, would the monkeypox outbreak have been covered so closely? Of course, COVID-19 shone a spotlight on the infectious disease landscape that won’t go away anytime soon, but we must not forget the lessons learned when reporting emerging outbreaks – whether caused by novel pathogens or known offenders.
Public-facing science communication took a hit in the early stages of the pandemic (and persisted throughout), with misinformation polluting every corner of the Internet. Monkeypox and COVID-19 are not the same, but we must apply what we’ve learned to prevent rampant misinformation – and to avoid inciting abuse and stigma against specific groups of people.
For instance, so far, monkeypox has appeared to disproportionately affect men who have sex with men. Although susceptible populations must be educated to recognize the symptoms and prevent transmission, healthcare organizations and the media must be careful and balanced to avoid feeding prejudices against gay and bisexual men. The virus can affect anyone, regardless of sexuality – and scientists and doctors must ensure that they relay reliable, scientifically correct information and limit the spread of misinformation.
- Centers for Disease Control and Protection (2022). Available at: https://bit.ly/3msQyGd.
- David Jinks Milt (2022). Available at: https://bit.ly/3MAyJj1.
During my undergraduate degree in psychology and Master’s in neuroimaging for clinical and cognitive neuroscience, I realized the tasks my classmates found tedious – writing essays, editing, proofreading – were the ones that gave me the greatest satisfaction. I quickly gathered that rambling on about science in the bar wasn’t exactly riveting for my non-scientist friends, so my thoughts turned to a career in science writing. At Texere, I get to craft science into stories, interact with international experts, and engage with readers who love science just as much as I do.















