
Painful Inequality?
How sex-dependent differences in molecular mechanisms could underpin men and women's distinct experiences of chronic neuropathic pain.
For the first time, researchers have used RNA sequencing to demonstrate key differences in chronic pain manifestation between men and women, driving a major rethink about the molecular mechanisms at play (1, 2, 3)
Theodore Price, Eugene McDermott Professor of Neuroscience at The University of Texas, is one of the lead researchers involved in the study, which pioneers the use of human dorsal root ganglion (DRG) samples – a major shift for the field. “There are limitations to traditional animal models for these kinds of studies,” he says. “Our new paper has driven a large foray into molecular neuro-biology in patient samples. It’s really been enabled by the RNA sequencing revolution in biology, which has been extraordinarily informative in our work.”
In partnership with clinicians at the MD Anderson Cancer Center in Houston, the team recovered DRG samples routinely removed as part of surgical procedures used to treat spinal cord tumors. “When you remove parts of the spinal column during these surgeries, you need to put in some kind of synthetic support to ensure mechanical function is retained,” explains Pradipta Ray, a research scientist involved in the project. “This process often requires that surgeons excise DRG’s in the region – for the most part these are healthy, non-cancerous tissue samples that are otherwise simply being thrown away.”
The researchers were keen to make the most of a unique opportunity. “Utilizing thorough data-sets provided by the team at MD Anderson, we were able to segregate our DRG samples into two groups – those mapping to a part of the body where patients had reported neuropathic pain, and those where they had not,” says Ray. And the results were unexpected: “Though we verified many mechanisms that have already been identified in mouse models, we also found upregulation of a range of genes thought to be involved in neuropathic pain unique to the DRG samples,” says Price.
One such strongly upregulated gene in the patient samples was Oncostatin M (OSM) – a key regulator of the interleukin-6 (IL-6) signaling pathway, which plays a key role in tissue inflammation. In fact, IL-6 sequestering approaches have been trialed – with limited success in the clinic as a therapy for chronic pain (4). Their failure, Price suggests, could be down to mistargeting. “I can’t help but wonder if perhaps IL-6 plays a more important role in rodents than it does in humans, and inversely with OSM in humans,” he says. “OSM has another co-receptor – GP130 – which is part of the same family as IL-6. And that’s where the failure to translate may have stemmed; the signalling and receptor pathway was correct, but the ligand was different between species.”
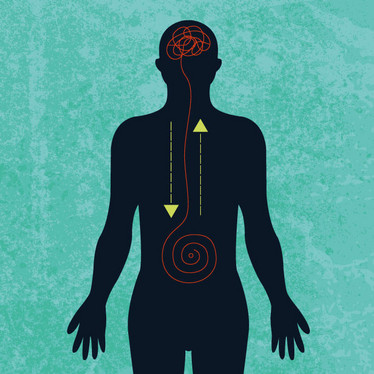
But the most striking finding is that RNA transcriptome profiles of male and female chronic pain sufferers are different – implying different pathways to pain. For Price, this wasn’t entirely unexpected. “Over the last few years, an idea has emerged about sex differences in neuropathic pain, based on models in mice,” he says. “The thought was that microglia and macrophages are key drivers of neuropathic pain in male mice, but not in females.” For the first time, however, those same differences have been reflected in human’s samples.
Though certainly encouraged by the findings, Ray is cautious about extrapolating too much from the results – at least for now. “We’ve been able to find signaling pathways we can associate with inflammation and pain with the fos-jun transcription program in males that is not reflected in females. But we have to remember that this wasn’t a controlled experiment – the transcriptional responses in these patients are happening at different points in time because we are sampling these patients DRG’s at different phases of the pain response,” he says.
Recognizing the need for more data (Price notes that, since the publication of the paper, the team have sequenced a further 20 samples), Ray is excited by the opportunity to further explore the differences: “We’re particularly interested in understanding the immune response in DRG’s because it’s dependent on three sources – innate immunity, resident immune cells, and infiltrating immune cells. We’d like to try and get a clearer handle on whether or not there is some kind of immune invasion from non-resident macrophages or t-cells,” he says.
According to the team, the ultimate goal is to allow clinicians to determine sub-types of chronic neuropathic pain (based on the immune profile of the DRG) to allow more precise therapeutics. “Starting with the actual human data has huge advantages – we have a much better chance of finding an effective therapeutic, if we know its target is present in humans rather than rodents,” says Ray.
The researchers are also seeking tests that may be more applicable in a clinical setting. “We are working with hospitals to gain blood samples from chronic pain patients to see if there are correlated biomarkers between the DRG and the blood,” Ray explains. “Blood sampling is considerably less invasive, as well as being much more rapid; we want to see if we can use it as a proxy for changes happening in the DRG.” By digging further into the “fine details” while investigating the potential for clinically relevant tests, the team are hoping to pave the way to better pain diagnostics and, ultimately, more targeted therapeutics to ease the pain of patients – both men and women.
Price is also confident in the approach. “The mouse is a good model to try and understand basic neurobiology,” he says. “But the fine details are actually quite divergent.” To unpick those details, the team hopes to develop a more robust model of the disease, taking into account the contribution of numerous biological factors: “We need to remember to look at the bigger picture, both in terms of neuronal physiology, but also the glia, the immune cells, and the cross talk between them all,” says Ray.
Such an approach will require the adoption of large data processing capabilities. Could machine learning technology prove key? “Using a model called Random Forest (5, 6) we’ve been able to achieve 94 percent accuracy in classifying our samples correctly in terms of their pain and sex state. The challenge now is to scale that model, and move from a purely descriptive model towards one that highlights why samples are different; for example, by highlighting particular patterns of signal regulation,” says Ray.
- RY North et al., “Electrophysiological and transcriptomic correlates of neuropathic pain in human dorsal root ganglion neurons,” Brain, [Epub ahead of print] (2019). PMID: 30887021.
- PR Ray et al., “Transcriptome Analysis of the Human Tibial Nerve Identifies Sexually Dimorphic Expression of Genes Involved in Pain, Inflammation, and Neuro-Immunity,” Front Mol Neurosci, 12, eCollection (2019). PMID: 30890918.
- PR Ray et al., “Comparative transcriptome profiling of the human and mouse dorsal root ganglia: an RNA-seq-based resource for pain and sensory neuroscience research,” Pain, 159, 1325-1345 (2018). PMID: 29561359.
- YQ Zhou et al., “Interleukin-6: an emerging regulator of pathological pain,” J Neuroinflammation, 141, eCollection (2016). PMID: 27267059.
- SJ Rigatti., “Random Forest,” J Insur Med, 47, 31-39 (2017). PMID: 28836909.
- [An explanation in more layman terms] N Donges, “The Random Forest Algorithm,” Towards Data Science, available at: bit.ly/2u7erIB Accessed 26 April 2019.
















