From MS to AMR
A 20-year-old drug used to treat symptoms of MS could be repurposed to treat infections in cystic fibrosis patients
A 20-year-old drug used to treat symptoms of MS could be repurposed to treat infections in cystic fibrosis patients
The immunomodulator glatiramer acetate (GA) has been used to treat multiple sclerosis patients for over 20 years. The drug is well tolerated by most patients, can be administered systemically – but why would it be effective in the fight against antibiotic resistance? We spoke to co-author of a study into its antimicrobial effects (1), Thomas Vorup-Jensen, professor at the Department of Biomedicine, Aarhus University, Denmark, to find out more…
Why did you choose to investigate glatiramer acetate as a potential antimicrobial agent?
We have worked for many years on the effects of GA in multiple sclerosis, and we noted that its biochemical properties are similar to the so-called antimicrobial peptide, LL-37. In spite of their name, antimicrobial peptides often exert a modulatory effect directly on the immune system without the involvement of microbes. In a previous paper (2), we compared the effects of GA and LL-37 on human immune cells and concluded that certain effects of LL-37 were also found in GA, suggesting that GA affected the immune system in ways mimicking the evolutionary highly conserved LL-37.
Then we asked the question that is central to this more recent study: if GA mimics the immunomodulatory effects of LL-37, could it also mimic the antimicrobial effects?
And the answer?
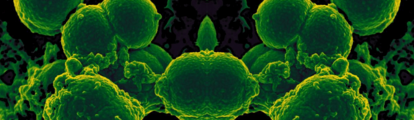
GA efficiently kills Gram-negative bacteria, in particular Pseudomonas aeruginosa, which is a crucial finding, as we lack antibiotics/antimicrobials that target these organisms; many Gram-negative organisms develop multiresistance to conventional antibiotics. As GA is already in use, we have the opportunity to repurpose it as an a new treatment of Gram-negative infections. Finally, we argue that the Gram-positive organism Staphylococcus aureus, presumably by shedding fragments of its thick cell wall, generates a type of nanoparticulate decoy that may deviate the attack of GA or LL-37, which may explain why S. aureus is better at surviving treatment with GA and LL-37 than the Gram-negative organisms.
Where could GA have the most clinical impact?
Cystic fibrosis patients in particular have trouble clearing bacterial infections from their lungs, very often infections with Pseudomonas. We hope that our discovery will help fight these infections in a more effective way.
What’s next?
We want to understand the mechanisms of GA killing better. We also want to investigate the effects of GA on other bacteria, with the aim of hopefully expanding the number of clinically significant infections which can be treated with this compound.
- SH Christiansen et al., “The immunomodulatory drug glatiramer acetate is also an effective antimicrobial agent that kills Gram-negative bacteria.”, Sci Rep, 7, 15653 (2017). PMID: 29142299.
- SH Christiansen et al., “The random co-polymer glatiramer acetate rapidly kills primary human leukocytes through sialic-acid-dependent cell membrane damage”, Biochim Biophys Acta, 1859, 425–437 (2017). PMID: 28064019.

I have an extensive academic background in the life sciences, having studied forensic biology and human medical genetics in my time at Strathclyde and Glasgow Universities. My research, data presentation and bioinformatics skills plus my ‘wet lab’ experience have been a superb grounding for my role as a deputy editor at Texere Publishing. The job allows me to utilize my hard-learned academic skills and experience in my current position within an exciting and contemporary publishing company.















