Decoding Depression
The publication of over 100 genetic markers associated with depression has rocked the neuroscience community. Here, we sit down with one of the authors to find our more.
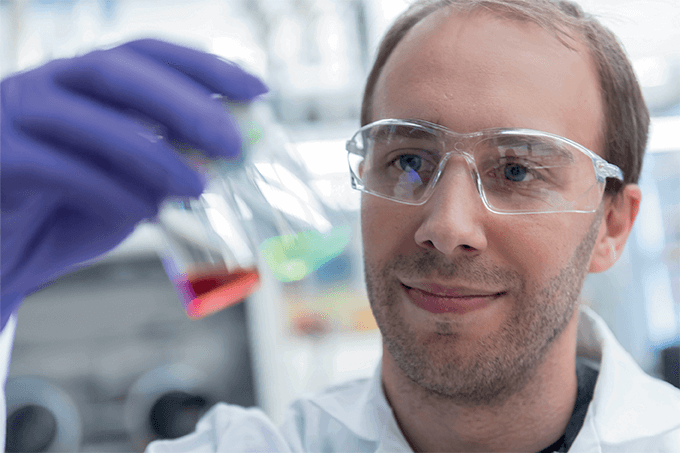
A paper published in Nature Neuroscience highlights 102 genetic markers associated with depression (1) – and it’s generating a great deal of excitement within the scientific community and beyond. Here, one of the papers co-authors – David Howard, Postdoctoral Research Fellow at the University of Edinburgh, Scotland – tells us more about the pioneering work.
What events led to the paper?
Over the last five years there has been huge progress in understanding the genetics of depression. Various different groups have all been working on their own studies – including initiatives such as the UK Biobank. Our group, based in Edinburgh, had initially elected to study depression in that particular cohort. Around the same time, there was an effort by the Psychiatric Genomics Consortium, which analyzed data from 35 different cohort. We decided it would be good to combine the results from both sources. It’s taken the past year or so to work through all that data – and it all culminated in the paper published in February 2019.
We show in our paper that depression has a definite risk component that is dependent on genetics. Of course, there are other factors – not least prior and current life experiences – that influence the development of depression, but the genetic component is clear – and it’s detectable.
After isolating roughly 100 positions on the genome that are associated with depression, we were able to access a brand new cohort – not yet fully available – from 23andMe. They looked up the variants we’d identified in our studies, and compared them with people who had self-reported a clinical diagnosis of depression. It turned out that all the variants moved in the same direction; that’s like flipping a coin 100 times and getting “heads” every single time – quite remarkable! Inspired, we performed some statistical analysis and found that, in fact, 87 of our 102 variants were significant in the 23andMe cohort. Obtaining the same signals in these different cohorts really suggests to us that our initial findings are robust.
What happened next?
After identifying the genetic variants for depression, we wanted to understand what they were likely to control biologically. We looked broadly – at the kidneys, the gastrointestinal tract, and so on – but the one that really stood out for us (perhaps unsurprisingly) was the central nervous system. And that drove further analysis of brain regions in more detail, which highlighted the frontal regions – the frontal cortex and the interior cortex (the “thought” bits of the brain) – as being particularly important.
A proportion of the genetic component for depression was shared with other traits too – most notably psychiatric disorders, including bipolar disorder and schizophrenia, but also other things, such as morphological traits, including obesity, a tendency towards overweightness, inflammatory bowel disease and Crohn’s disease. Insomnia and a host of sleep-related conditions were also highlighted. And that’s not really surprising – if you look at people who are clinically diagnosed with depression, common questions from clinicians include, “Has your weight changed?” or “Have your sleep patterns altered?” It’s interesting to see how clinical assessments match up with the shared genetic architecture between depression and those conditions.
How might your findings be applied?
Not everyone who has depression has the same symptoms – it’s quite heterogeneous in that regard. So the next stage is trying to stratify types of depression with the support of genetic information, which could allow us to treat the symptoms most typically associated with those types. For example, genomics might help us understand whether someone would benefit from pharmacological or psychological interventions.
Reviewing the medical literature, we looked at the interactions between genes that play a role in depression and a list of commonly prescribed drugs. As expected, one of the key dopamine receptor genes had a lot of interactions with a class of anti-psychotic and anti-anxiolytic drugs. It was also exciting to find 54 other drug classes that have an influence on these depression genes. Clearly, we need to be careful about extrapolating too far at this early stage, but one of the big drug classes was a branch of chemotherapeutic agents. We know that some cancer treatments have depressive effects on people – and our work potentially explains why; the drugs used to treat cancer might be interacting with these genes. Conceptually, by scanning the genomes of cancer patients, we could try to reduce the risk of depression by offering drugs that don’t interact with those particular genes.
Over the next 5–10 years, I think that we’ll see similar links across a lot of other disorders. But trying to make the jump between associated genes and what’s useful in the clinic will be a small-step process!
Much further down the road, we’ll likely be able to collect a wide range of biomarkers or genetic information for everyone. DNA sequencing technologies are getting cheaper and cheaper, and, in the future, general practices will hopefully be able to take a sample of your blood or saliva and extract your DNA, putting on record anything that could be informative at a later date. Being able to stratify patients and their diseases in this way would be powerful indeed. Our paper is just one of those small steps towards that future.
- DM Howard et al., “Genome-wide meta-analysis of depression identifies 102 independent variants and highlights the importance of the prefrontal brain regions”, Nat Neurosci 22, 343–352 (2019). PMID: 30718901.