Lessons I’ve Learned
From being one of the first clinicians to voice doubts over Vioxx, to his latest book calling for a complete transformation of the patient–doctor relationship, Eric Topol has never been afraid to raise his head above the parapet. Here, he describes what he’s learned from life as a clinician–researcher and his current role as Director of the Scripps Translational Science Institute.

I never want to stop seeing patients
I didn’t grow up wanting to be a doctor; I was set on being a scientist. I studied genetics at college and published a thesis called “Prospects for Genetic Therapy in Man” in 1975; it took 40 years before gene therapy became a reality! But in my third year at the University of Virginia I took a job working nights in the hospital, and seeing the staff help people get their health back on track made me decide that being a clinician would be a great career.
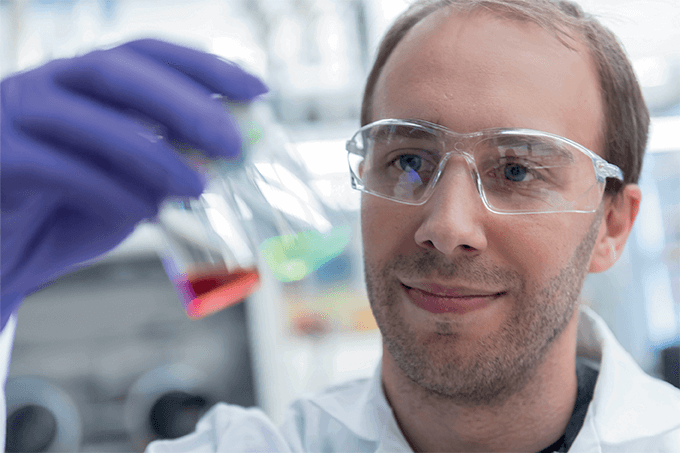
I never lost my interest in research though. Even as a medical student, I found time for some research and since I finished medical school in 1979, I’ve always integrated research with patient care. I don’t think I could do good clinical and translational research if I didn’t still look after patients. You need to have a pulse on what it is like to be a patient and a doctor today, to understand the unmet needs and opportunities.
My research interests have evolved over time, but the end goal has always remained the same

During my fellowship in 1984, I got to treat the very first patient with recombinant human tissue plasminogen activator (tPA), which sparked my interest in biotechnology and genetic engineering; I worked for several years on treatment of acute heart attacks. By the mid-90s, I had a growing realization that no treatment for acute heart attack is going to substantially improve outcomes; by the time the patient reaches us, they are at least a few hours into the event and a lot of heart muscle has died.
I decided it was time to redirect my energies into preventing heart attacks, and that took me back to my longstanding interest in genetics. In the late 90s, I put together a very large cardiovascular gene bank, including DNA and electronic health records of 10,000 patients, which led to discoveries of gene variants associated with heart attacks. From there, my work broadened to encompass not just cardiology but all sorts of diseases with a genetic component – from sudden death to cancer.
In the past decade, my work has evolved again as technology has advanced to a point where it is feasible to look well beyond genomics. We can record so much data through smartphone sensors, lab tests and imaging, that we now have a way to understand the granular aspects of each individual and see them as “high-definition human beings”. It is really exciting.
Scripps Translational Science Institute is unique
I think we were the first to take a “panoromic” approach. Some translational research centers specialize in genomic research, while others focus on digital medicine. But we aim to integrate multiple layers of information for building the “individualome”. Biosensors capture the physiome, scans map out anatomy, we can analyze the genome, proteome, epigenome, metabolome and microbiome, and then of course there is the exposome - the environment, which can be quantified by sensors. We truly believe we can digitize just about anything, and over the past nine years we have got better and better at it. Of course, that generates an awful lot of data, but we are fortunate to have a really great bioinformatics analytical team, led by Ali Torkamani, and a partnership with the San Diego Super Computer Center. San Diego is a real hotbed for both genomics and digital medicine, so we have the right people, the right place and the resources at hand – it’s a dream come true for me.
The secret to a long and healthy life is a mystery, but it’s not unsolvable
A project we’re working on at Scripps that I’m particularly excited about is looking at how long you remain healthy – the “health span” – as a phenotype. I often state that healthy aging is 100 percent due to genetics and 100 percent due to your environment. In other words, the different factors are so tightly intertwined that you can never really sort out each component quantitatively for any individual. When you see a 99-year-old who smokes two packs of cigarettes a day and has never been sick, you have to assume genetics plays a part. But when you see someone who is 104 and still driving a car, and find out that their parents died at a very young age, it is clear that genetics isn’t the whole story either. What is exciting is that we now have the tools to start to unravel the mystery.
We have collected a wealth of omics and other information on an extraordinary group of people who – at an average age of 90 – are still active, healthy, and take no medication. We call them the “Wellderly”. There has been some research on the factors affecting lifespan, but we believe living a long, healthy life is an essential – and perhaps more valuable – phenotype for study. Longevity can be extended with many medical interventions, making it “unnatural”, whereas healthspan, as we’ve defined it, is an arc of human nature. It took eight years to complete our study, from recruiting participants to genome sequencing and a range of other analytics, and we hope it will be the first of many studies to begin to unravel the factors affecting health span.
Medicine isn’t working

I called my first book “The Creative Destruction of Medicine”, referencing a term coined by economist Joseph Schumpeter. Current medical practice is a failed model – it’s expensive, wasteful and imprecise. We have too many patients undergoing screening and interventions that are unnecessary, while others aren’t diagnosed until a late stage of disease, if they receive a diagnosis at all. There are over 12,000,000 serious medical errors per year in the USA and that figure hasn’t really changed in 15 years.
I believe we now have an extraordinary opportunity to re-boot how medicine is practiced by adopting individualized medicine, and giving patients more control. It’s there for the taking – but only if doctors and patients embrace it.
Smartphones and wireless devices are already changing medicine
I’m a cardiologist, but I haven’t used a stethoscope for over five years now. Instead, I use a high-resolution hand-held ultrasound probe, connected to my smartphone, to see the heart in action. It’s one of the most extraordinary devices I have ever worked with – I can show patients the footage in real-time, and send them the video in case they need a baseline for comparison in future. I can also do an electrocardiogram with each patient in my clinic, using a credit card-size device linked to my smartphone.
Another device I would really like to see validated and in clinical use is a watch-like device that takes your blood pressure with every heartbeat. This is a big unmet need since high blood pressure is one of the most common chronic medical conditions and most people don’t have it very well controlled. We have never been able to unobtrusively measure blood pressure continuously throughout the day and night, so this could provide us with a wealth of new information.
The doctor’s appointment of the future will be very different to today
You will be more likely to talk to your doctor online than in their office, and the focus will be on data exchange. Your omics and other data will be analyzed, interpreted and visualized by algorithmic machine learning or artificial intelligence, so the doctor can summarize and offer guidance.
Let’s say a test has detected cancer, and you need to know what treatment approach will work best. Your doctor is no longer reliant on published research, instead he or she can mine information from millions of people and match you up with those whose demographics, genome and sensor data are most similar to yours, to find out what treatment has worked best for them. You are effectively being matched with your virtual “identical twins”.
Clinicians are resistant to change
I believe we are facing the biggest challenge in the history of medicine. It’s not just about digitizing information, but about control and power. Doctors are notoriously conservative. They have reimbursement models to contend with, and many find the idea of ceding authority difficult.
I strongly believe that doctors underestimate their patients’ ability to handle their data and medical information in general. Are some people going to obsess about their data? Of course. But all the studies I’ve seen and we’ve done indicate that the vast majority of people handle having access to their data really well, even when it suggests bad news.
Think big, act bigger
When you stir up some controversies, there will always be people who disagree or misinterpret what you are trying to do. I try to just keep my head down and get it done – with the help of my incredible team. I’m no fanatic – I’m just trying to push the field forward.


Eric Topol is Director of the Scripps Translational Science Institute, CA, USA.